A method known as CRISPR allows scientists to edit the DNA of living organisms. A recent paper shows that this method can be used to restore hearing in adult mice with a form of genetic deafness.

Image by Pexels
Perhaps you have heard DNA referred to as the “blueprint for life.” Indeed, DNA contains the instructions needed to build and maintain all living organisms. It determines everything from the scent of a flower, to the color of a dog’s fur, to a person’s height. But what happens when there are mistakes in this blueprint?
Some mistakes, or mutations, can be completely benign, but others can have disastrous effects, leading to diseases like sickle cell anemia and cystic fibrosis. For cases like these, scientists have been developing treatments known as gene therapy. One form of gene therapy is known as gene editing. This technique allows scientists to actually change the DNA of a living organism, as if they were correcting mistakes in a blueprint. A recent paper shows that one type of gene editing, CRISPR, can be used to restore hearing loss in adult mice.
CRISPR gene editing uses two main components, a guide RNA (gRNA) and a Cas protein. Once these components are delivered into a cell, the gRNA guides the Cas protein to the precise portion of DNA that needs to be edited. The Cas protein then cuts the DNA at this spot. Once the DNA is cut, scientists can employ one of two methods to edit the gene. One option is to insert a new piece of DNA at the break. In this way, scientists can replace a disease-causing mutation with a healthy sequence of DNA. The second option is to allow the cell to naturally repair the DNA break through a mechanism known as non-homologous end joining (NHEJ). This mechanism essentially glues the two severed ends of DNA back together, but is often error-prone, adding or deleting pieces of DNA in the process. Therefore, if NHEJ occurs in a portion of DNA containing a gene, the gene will often be turned off or disabled. Scientists can use CRISPR in this manner to turn off disease-causing genes.
Both of these methods for using CRISPR show immense promise for the treatment of various genetic conditions, many of which currently have no cure. One such condition is hearing loss. Around half of hearing loss cases can be attributed to genetic causes, but there is no treatment that reverses or even slows down genetic deafness. Previous studies have used gene editing methods to restore hearing loss in newborn mice, but mice are born with immature structures in their inner ear. Human newborns, on the other hand, have fully developed inner ears. How might gene editing methods tested in mice help with human hearing loss then? Zhu and colleagues investigate this question and demonstrate how CRISPR can be used to restore hearing loss in adult mice with fully developed ears as well.
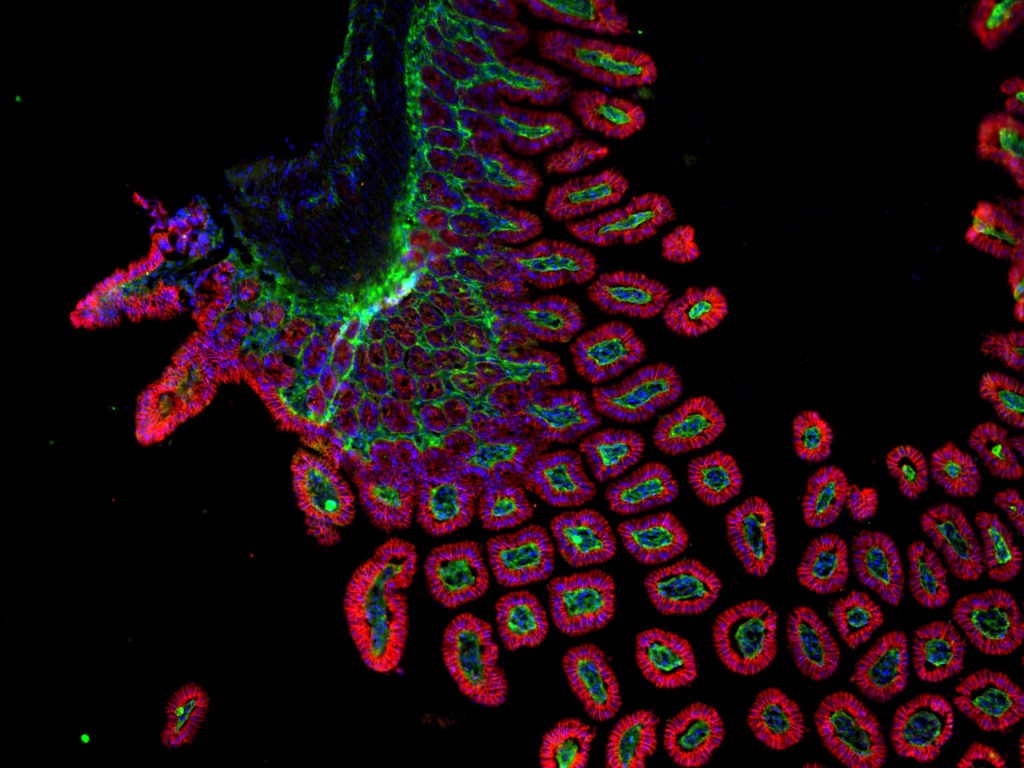
In their research, the scientists focused on a form of deafness attributed to mutations in a gene called MIR96. This gene encodes a microRNA (miRNA), a short RNA molecule that helps cells to regulate the types and amounts of protein they produce. In the inner ear, miRNAs play an important role in development and are required for normal hearing. Specifically, MIR96 is required for normal development of hair cells, which sense sound and are vital for hearing. In humans, mutations in MIR96 lead to autosomal dominant deafness-50 (DFNA50), and similarly, Mir96 mutant mice exhibit hearing loss starting at 4 weeks old and progressing by 8 to 12 weeks old. Mutant mice also display abnormal hair cells in addition to an overall reduction in the number of hair cells present during development.
In this specific study, the researchers sought to use CRISPR to restore hearing in the Mir96 mutant mice by designing a gRNA to target the mutant version of Mir96. When injected into the inner ears of mutant mice along with a Cas protein, the gRNA guides the Cas protein to mutant versions of Mir96. The Cas protein then cuts the DNA of the mutant gene, and NHEJ occurs, disabling the faulty gene in many cases. In this way, the scientists can effectively turn off the mutant Mir96 gene in the inner ear.
The key to this study was that scientists only applied CRISPR to one ear – the other ear was left untouched to serve as a control. The mice were first injected at 6 weeks old, after typical onset of hearing loss. While the uninjected ears developed hearing loss as expected, the injected ears showed an improvement in both short and long term hearing. Additionally, CRISPR treatment also improved hair cell survival and structure in the injected ears compared to the uninjected ears.
To assess whether treatment was effective at different time points, the researchers also treated mice at 3 weeks old, when hearing loss was detectable only at high frequencies, and at 16 weeks old, when hearing loss was already severe. Animals injected at 3 weeks old showed even greater improvements in hearing than the mice injected at six weeks old. However, the mice injected at 16 weeks old showed no significant improvements in hearing. These results indicate that early intervention works best, and that intervention is not effective once hearing loss has reached severe stages.
Given these promising results, the scientists continued by performing a safety assessment. The goal was to address whether the CRISPR treatment had any unintended side effects and to make sure that the CRISPR machinery edited only the intended Mir96 mutation and not any unintended (off-target) sites. They not only found that the treatment was safe, but also that it had negligible off-target effects.
To translate their findings to humans, Zhu and colleagues used the same gRNA from the mouse experiments as well as two additional gRNAs designed to target two additional MIR96 mutations. They delivered the three gRNAs, with Cas protein, into human cell lines containing the three MIR96 mutations. Each gRNA successfully disrupted its corresponding MIR96 mutation, suggesting that similar treatment could be effective in treating human hearing loss.
While many more studies will be necessary before these findings are developed into a clinical treatment for genetic deafness in humans, this paper provides a valuable proof-of-concept that gene editing is able to reverse hearing loss in adult animals. If DNA is life’s blueprint, then CRISPR is the ultimate red pen — crossing out errors and rewriting a second draft.
Edited by Emily Faulkner & Jayati Sharma

Leave a comment