A new study by Chawla et al. characterized changes in DNA openness associated with major depressive disorder in human brain samples. They identified cell type-specific changes and linked genetic variants to changes in gene expression.

Major depressive disorder (MDD) is a globally common mental health disorder that can be extremely debilitating. As of 2021, more than 8% of adults and over 20% of adolescents in the United States had experienced at least one major depressive episode within the previous year. People dealing with MDD experience an ongoing low mood and lose enjoyment from activities they previously enjoyed. While we don’t fully understand all of the factors that contribute to MDD, it seems to be caused by a combination of biological, environmental, and social factors. As such, researchers continue to work towards uncovering the mechanisms that contribute to its development.
Some scientists have used genome-wide association studies (GWAS, for example these studies and analyses by Howard et al., Meng et al., and the Major Depressive Disorder Working Group of the Psychiatric Genomics Consortium) to identify genetic variations that occur more frequently in individuals with depression, in hopes of finding genetic factors that can lead to the disorder. However, just identifying that a variant is associated with the disorder doesn’t tell us how the variant contributes to depression, or whether it even truly causes depression at all. Additionally, variants identified by GWAS often don’t occur in genes that code for functional proteins, so it can be difficult to figure out what their impacts might be.
Another important layer of genetics beyond just the sequence is whether particular regions of the genome are tightly compacted (closed) or “unwrapped” (open), since genes need to be accessible to cellular proteins in order to be expressed. Genetic variants in regions that are involved with regulating DNA openness may lead to altered accessibility of certain genome regions, thus potentially allowing some genes to be used more or less than usual. These changes in the DNA that don’t impact the sequence are epigenetic changes. Depending on what genes are affected, there could be health consequences.
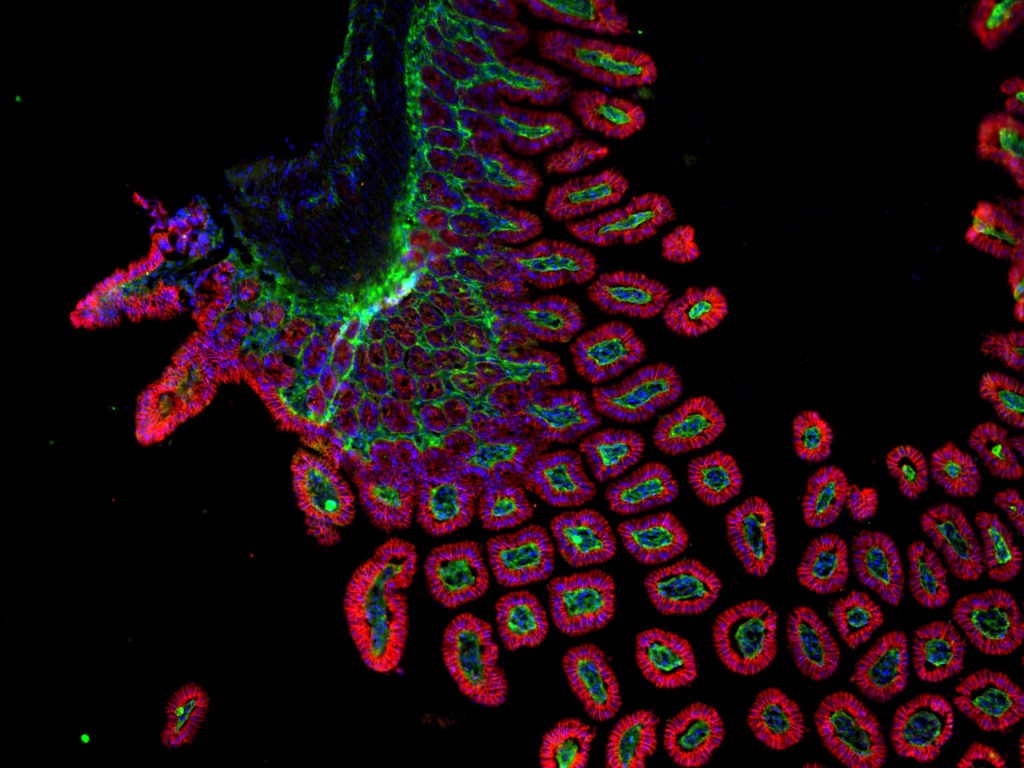
One technique that scientists use to study the accessibility, or openness, of DNA regions is called Assay for Transposase Accessible Chromatin with high-throughput sequencing (ATAC-seq). In ATAC-seq, an enzyme adds short DNA adaptor segments into open genomic regions. These adaptors allow scientists to selectively sequence the open regions, which allows them to pinpoint where in the genome those open regions are. Since DNA openness can affect how much a gene is used, knowing which genes are more or less open in patients could offer insight into gene expression patterns contributing to depression.
In a recently-published Nature Genetics study, scientists profiled the accessibility of the genome in brain cells from 44 individuals with MDD who died by suicide and 40 individuals without the disorder using single-nucleus ATAC-seq. This assay allows scientists to map out the openness of DNA from nuclei of individual cells, rather than mapping indiscriminately from a bulk population of cells, so they can look at similarities and differences between different cell types. They found that out of all the regions with different openness in MDD vs. non-MDD cells, most of the regions were less open in MDD compared to non-MDD. Using computational analysis, the researchers also found that regions that had altered openness in the MDD samples were likely to be linked to genes that were expressed differently in the same cell donors.
One group of excitatory neurons [a cluster of deep-layer NR4A2+ excitatory neurons] that had over 20% of the regions with different openness were also enriched for heritable risk of MDD, based on data from previous studies. In the same cell type, transcription factors (proteins that regulate gene expression) that were likely to be able to bind within differently open regions included some that were previously associated with heritability of MDD.
Using multiple computational tools, the researchers identified 97 MDD-associated genetic variants that are likely to impact region openness in particular brain cell types. Incorporating several other sources of relevant genetics-related data, they found that 25 of these showed an effect in the same neuron type discussed above. Some of these variants had been previously associated with psychiatric disorders, and 10 of them were associated with differential openness only in this cell type.
Another type of cell that showed a lot of differentially open regions was a cluster of microglia, which are immune cells in the central nervous system. These cells exhibited a genetic profile enriched for genes expressed by grey matter microglia, which were previously shown to have differences in gene expression in MDD brain samples. One genetic variant associated with MDD in these cells that had an allelic effect on openness (an effect from the specific version of the gene) is known to disrupt a binding site for a transcription factor.
Since a lot of this analysis centered around genetic variants previously associated with MDD, you might wonder, what makes this study uniquely valuable? Well, if we can understand how MDD-associated variants exert their effects, we can design ways to counter their contributions to depression. This study revealed cell type-specific effects, which are important to consider when designing treatments; after all, there’s a lower risk of unintended effects if we can target only the cells where there’s a problem. Additionally, with big genomic datasets, multiple research groups with different specific questions can analyze the data in different ways. While additional cell- and animal-based experiments would be needed to bring these findings to the clinic, the findings from this study can help scientists extend our understanding of the cellular changes that occur in this devastating disorder.
Edited by Mandy Eckhardt and Jayati Sharma

Leave a comment