Who needs something new when you can repurpose what you already have? A 2025 study finds that medications designed for cystic fibrosis and high blood pressure effectively resolve key physiological changes in a cell culture model of COPD and cigarette smoke exposure.

Doctors and public health officials frequently remind us how important it is to take care of our lungs. From stop-smoking campaigns to clean air initiatives, there’s a lot of effort dedicated to minimizing exposure to major risk factors for lung diseases. This effort is well-placed: one lung disease, chronic obstructive pulmonary disease or COPD, is the fourth leading cause of death worldwide. Smoking and air pollution exposure are primary risk factors for its development, and once it starts, there’s no cure, only symptom management. Finding a new treatment option could be life changing for patients.
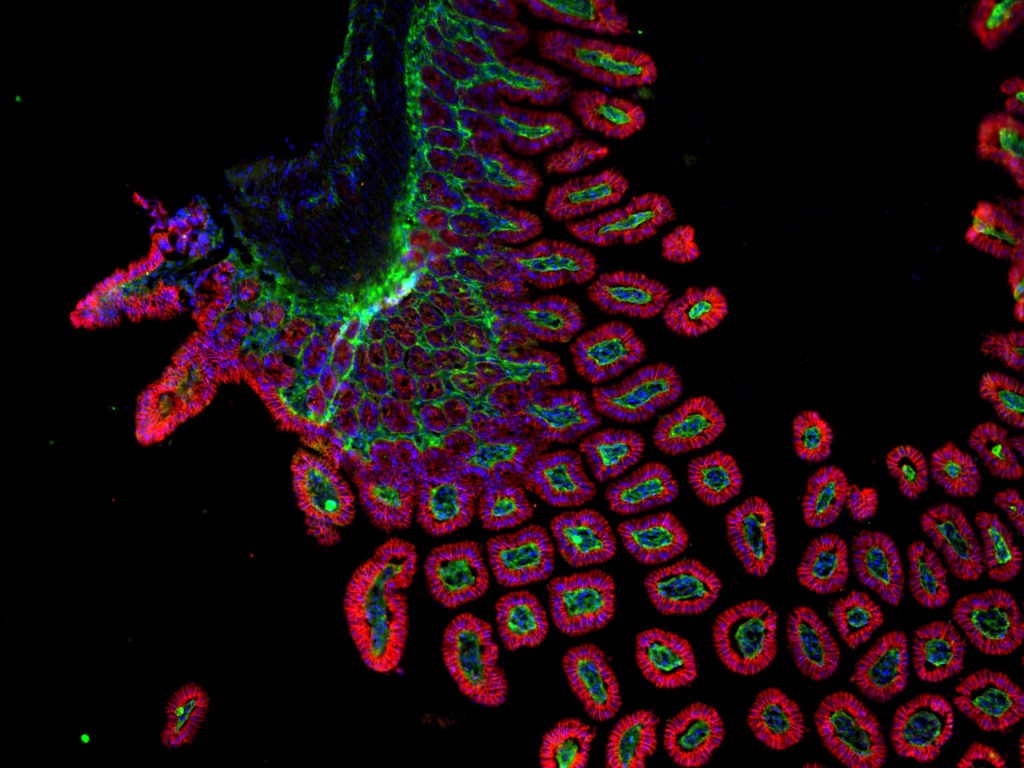
People with COPD can experience symptoms with a range of severity. Early-stage COPD may have minimal impact on the patient’s quality of life, requiring little more than the use of rescue medications during flare ups, while late-stage COPD patients are unable to function without supplemental oxygen, losing nearly all quality of life. One of the key factors behind this progression is airway inflammation. Persistent inflammation causes significant irritation of the airways, which respond by increasing the production of mucus. The goal is for the mucus to trap whatever is causing the irritation, so ciliated cells lining the airways can sweep the irritant out of the lungs using their hair-like protrusions. Typical mucus is mostly water, making it easy to push out of the lungs so it can be harmlessly swallowed or coughed out. However, in an irritated airway that produces too much mucus too quickly without the appropriate amount of water, the delicate cilia get weighed down and can’t sweep it out. This leads to mucus buildup, which narrows the airways and can even completely block airflow to parts of the lung.
Mucus buildup isn’t specific to just COPD. The major symptoms of another lung disease, cystic fibrosis (CF), are triggered by the extraordinarily thick mucus that patients produce. CF is caused by mutations in the CFTR gene, which normally produces a protein that helps control the amount of water added to the airway mucus to keep it thin enough for cilia to move. Common mutations in CFTR prevent the protein from reaching its designated spot at the cell membrane, which in turn prevents enough water from crossing the membrane and mixing with the mucus. This leads to thick, too-sticky mucus similar to that seen in COPD.
Based on these similarities between COPD and CF, a new study by Silswal et al, asked if a drug designed to thin mucus in CF could do the same thing in a cell culture model of COPD. To answer this question, the authors grew cells collected from the lungs of healthy people and patients with COPD, creating a mucus-producing disease-relevant model kept in a dish. Healthy and COPD cells were divided into four groups: unexposed, exposed to cigarette smoke only, exposed to the CF drug only, or exposed to both cigarette smoke and the CF drug. The cigarette smoke exposure was meant to mimic a trigger that could cause a COPD flare up with viscous mucus production. Treating the cells with the CF drug, nesolicaftor, before smoke exposure successfully reduced mucus viscosity, reduced mucus production, and increased cilia movement compared to cells exposed to cigarette smoke without treatment, nearly to the same level of cells not exposed to smoke at all.
Following those promising results, the authors investigated how nesolicaftor caused this effect. It belongs to a novel drug class of mRNA amplifiers, which stabilize mRNA transcripts so that more protein can be produced before the mRNA is degraded. Nesolicaftor specifically binds to PCBP1, a protein that binds to the CFTR mRNA and stabilizes it so more CFTR protein can be generated. Silswal et al. discovered that nesolicaftor also increases binding of PCBP1 to LRRC26, which codes for a subunit of another channel protein, BK, which, like CFTR, is involved with mucus hydration. After treatment, the activity of both CFTR and BK was significantly increased, indicating more water was mixing with the mucus layer.
Nesolicaftor was not the only drug capable of these functions. Two medications from a completely different class of drugs called angiotension II receptor blockers (ARBs), used to treat high blood pressure, also stabilize PCBP1 binding to CFTR and LRRC26. These drugs work by blocking TGF-β1, a protein which is over-expressed in people with high blood pressure and prevents PCBP1 from binding to its target mRNAs, causing them to be prematurely degraded. Blocking TGF-β1 allows stabilization of CFTR and LRRC26 mRNA to occur and increases protein production back to normal levels. Because TGF-β1 signaling pathways are also activated after smoke exposure, the authors hypothesized that ARBs would function similarly to nesolicaftor in a cigarette smoking model. Indeed, the authors found that two ARBs, losartan and telmisartan, significantly reduced mucus viscosity and improved the cilia’s ability to clear it after cigarette smoke exposure. Both drugs accomplished this in the same way nesolicaftor did: by increasing the activity of CFTR and BK proteins.
Silswal et al. started with a medication designed for CF and ended with a drug approved for high blood pressure, both accomplishing the same goal of thinning out thick mucus. The authors end by specifically discussing telmisartan, which is purported to more effectively block TGF-β1 at the same therapeutic dose as losartan: “Telmisartan … is [an] easily available, cheap and safe ARB to use, therefore presenting it as a good therapeutic option in COPD patients.” Studies like this could bring medications with a proven record of being safe and well-tolerated to COPD patients in need of novel treatments.
Edited by Olivia Fish and JP Flores

Leave a comment