A 2022 study shows that an Alzheimer’s risk gene causes certain brain cells to mismanage cholesterol, which is needed to produce insulation for neurons. These defects, however, can be reversed through treatment with a drug designed to increase cholesterol transport out of cells.
Imagine two seemingly identical groups of mice are subjected to a test to evaluate their cognitive abilities. In this assessment, mice are placed into an apparatus containing two chambers connected by a tunnel. One chamber is open and brightly lit, while the other is covered and dark. The mice prefer the shelter provided by the covered chamber, but are placed into the open one to start. After each mouse is given time to acclimate to the setup, the tunnel to the covered chamber is blocked with a piece of paper. The mice are placed back into the open chamber, and the time that it takes them to remove the piece of paper and enter the covered chamber is recorded. This test is repeated for four days, and on the last day, the times from the first day are compared to those from the last day. If the mice learned effectively, their time should decrease from day one to day four, as this would suggest that they remembered how to move the barrier from day to day. In this scenario, this is the case for the first group of mice; however, the second group shows no time decrease, indicating defects in their cognitive abilities. Although these two groups of mice look identical, they have one very important difference. The second group of mice have been engineered to mimic the symptoms of Alzheimer’s disease (AD).
Specifically, these AD model mice have been designed to express a variant of the human gene, APOE. This variant, known as APOE4, has been associated with an increased risk of AD in humans. In fact, carrying one copy of this variant increases an individual’s risk of AD three to fourfold, while two copies increase the risk by eight to twelvefold. Nearly half of all individuals with AD carry at least one copy of APOE4; however, the mechanisms by which this variant increases AD risk are not fully understood.
A 2022 study seeks to answer this question by using the aforementioned AD model mice as well as data from postmortem human brains and lab-derived brain cell cultures. In this study, samples with one or more copies of APOE4 are compared to those with two copies of APOE3, the more risk-neutral variant of the APOE gene. Throughout the study, the researchers focus particularly on one cell type called oligodendrocytes. These cells are responsible for the production of myelin, a fatty sheath that insulates the long projections from nerve cells that carry signals and allow communication between neurons and other cells. These projections are called axons, and their myelination speeds up signal transmission, increasing the efficacy of the nervous system. This means that defects in oligodendrocytes could interfere with a neuron’s ability to send and receive signals.
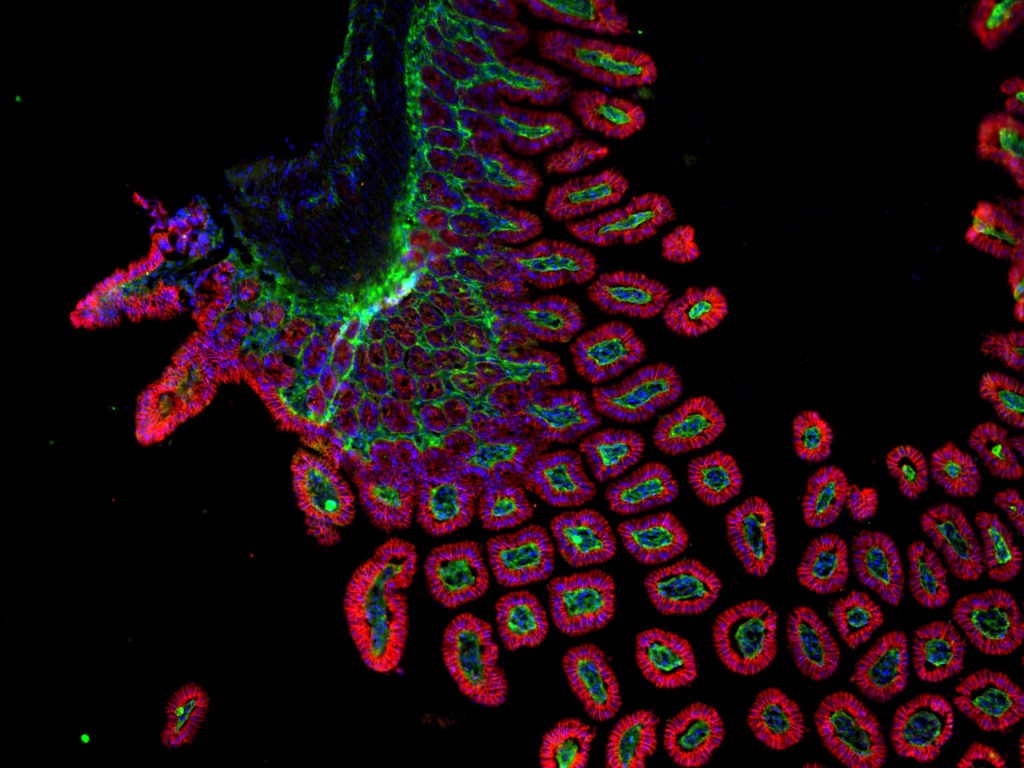
The researchers began this study by examining differences in oligodendrocytes from APOE4 and APOE3 postmortem human brains, using a technique called single-nucleus RNA sequencing (snRNA-seq). This procedure allows researchers to see exactly which genes are being used (expressed) in each cell of a given tissue, in this case postmortem human brains. Using this technique, the researchers found that, in APOE4 oligodendrocytes, expression of genes involved in cholesterol synthesis was increased, while expression of genes associated with cholesterol transport was decreased. This indicates that cholesterol could be accumulating in these cells rather than being shipped out of the cells. By directly visualizing the brain tissue using microscopy, they confirmed that cholesterol accumulates within oligodendrocytes in APOE4 carriers. These results were further confirmed using lab-engineered cell cultures of oligodendrocytes carrying either APOE4 or APOE3. In these cells, a form of cholesterol stored in lipid droplets within cells was increased in APOE4 cells compared to APOE3 cells. Additionally, when visualizing the oligodendrocytes using microscopy, the researchers found that cholesterol accumulates within the APOE4 cells, while, in APOE3 cells, it localizes mostly to the cell membrane. These findings suggest that cholesterol storage is increased in APOE4 oligodendrocytes compared with APOE3 oligodendrocytes.
Because cholesterol availability is the rate-limiting factor for the production and maintenance of myelin, the researchers hypothesized that the cholesterol abnormalities in APOE4 oligodendrocytes might lead to defects in myelination. To test this hypothesis, they first looked at the snRNA-seq data from postmortem human brains and found that expression of genes involved in myelination was decreased in APOE4-carrying oligodendrocytes compared to APOE3-carrying oligodendrocytes. Visualizing the tissue confirmed that APOE4 brains not only have fewer myelinated axons compared to APOE3 brains, but also have thinner myelin sheaths when myelination is present. The same results were found when the researchers examined tissue from the AD model mice. Together, these results suggest that carrying APOE4 leads to decreased myelination.
Therefore, all of this data elucidates a mechanism by which APOE4 leads to increased risk of Alzheimer’s disease. Carrying this variant leads to accumulation of cholesterol in oligodendrocytes, impairing their ability to myelinate axons. Based on this, the researchers asked whether these effects could be reversed using a drug, called cyclodextrin, that facilitates cholesterol transport out of cells. Interestingly, they found that treating APOE4 oligodendrocytes with cyclodextrin reduced intracellular cholesterol to levels similar to those of APOE3 cells. Also, when APOE4 oligodendrocytes were co-cultured with neurons, treatment with the drug increased myelination of the neurons’ axons. Similarly, in the AD model mice, treatment with cyclodextrin decreased cholesterol accumulation in oligodendrocytes and promoted myelination of axons. In fact, treatment of APOE4 mice not only increased the number of myelinated axons, but also the thickness of their myelin sheaths. These improvements in cholesterol transport and myelination also led to functional improvements in cognition, as APOE4 mice treated with cyclodextrin performed better than untreated APOE4 mice on learning and memory tests, such as the aforementioned puzzle box test. Therefore, pharmacological facilitation of cholesterol transport not only reverses the cholesterol and myelin defects seen in APOE4 mice, but also treats cognitive symptoms of AD.
Altogether, this study provides valuable evidence that cholesterol abnormalities in APOE4 carriers lead to defects in myelination. More importantly, the study also reveals a potential intervention to treat these defects. Perhaps, going forward, these results can inform future therapeutic interventions to treat and eliminate Alzheimer’s disease. The long awaited solution might be on the horizon.
Edited by Zach Patterson and Jameson Blount


Leave a comment