More than 10,000 rare diseases exist, affecting 30 million people in the United States. By combining science and human-centered design, we can conduct human-centered science that may help us find answers in the most obvious of places.

If we can design solutions for the most marginalized, we can extend these solutions to many. This is the core of human-centered design, an approach that involves the human perspective in all steps of the problem-solving process. The idea is that if you can design a solution for someone that is physically disabled and has one arm, for example, then this solution can be applied to someone with an injured or broken arm, or a parent that needs to use their arms to care for their newborn. Inclusive, human-centered design maximizes accessibility for the full range of human diversity and should be prioritized in the scientific process.
Rare diseases are essentially invisible in the healthcare system. In some cases, one individual may be 1 out of 200 in the world with a given condition. These conditions are often undiagnosed, leaving these patients and their loved ones looking for answers. More than 10,000 rare diseases exist, but there are only FDA-approved treatments for about 5% of them. This leaves a lot of room for impact, and by the principles of human-centered design, if we can treat the most marginalized of the healthcare system, perhaps these treatments can inform the mechanisms of diseases like Alzheimer’s Disease or cancer.
Many rare diseases are caused by the emergence of variants in a single gene. However, protein-coding genes only account for ~ 2% of the human genome, which begs the question— what is the role of the other 98% in the context of rare disease? It has become increasingly clear that this DNA dark matter plays a bigger role than previously thought.
Yuyang Chen, a DPhil student at the University of Oxford, wants to take an innovative lens to better understand rare disease genetics. Chen’s career started with doing experiments such as Western Blots, a staple experiment in molecular biology. He then moved into paleobiology, a field that looked into animal genomes for virus-related sequences. Now, he’s studying how the non-coding genome contributes to rare disease.
One of the many focus areas of the rare disease research community is diagnosing patients and decreasing their time on their ‘diagnostic odysseys’. As sequencing technology rapidly improves, Chen is interested in developing therapeutics to treat rare disease patients in the future. “For rare disease patients, around 80% have a genetic cause. You can actually find it in the genome, whereas in cancer or other diseases, it’s not as clear. You’d need to look at all sorts of data. You can look at transcriptomics or proteomics or other omics data.” Since most rare diseases are genetic, they’re more suitable for developing personalized genetic therapies for these patients compared to other diseases.
In July 2024, Nature released an unedited version of Chen’s work to give the rare disease community early access to his findings. Using data from Genomics England, a genomic healthcare company owned by the United Kingdom Department of Health & Social Care, he showed how certain genetic variants in the non-coding genome were more prevalent in patients with rare neurodevelopment disorders (NDDs) than in non-NDD individuals. “No one actually believed it at first!” Chen explained that these mutations were incredibly common in the NDD cohort, and he couldn’t believe that they haven’t already been discovered. Currently, there are very few effective ways to predict the effect or mechanism of rare variants in the non-coding genome.
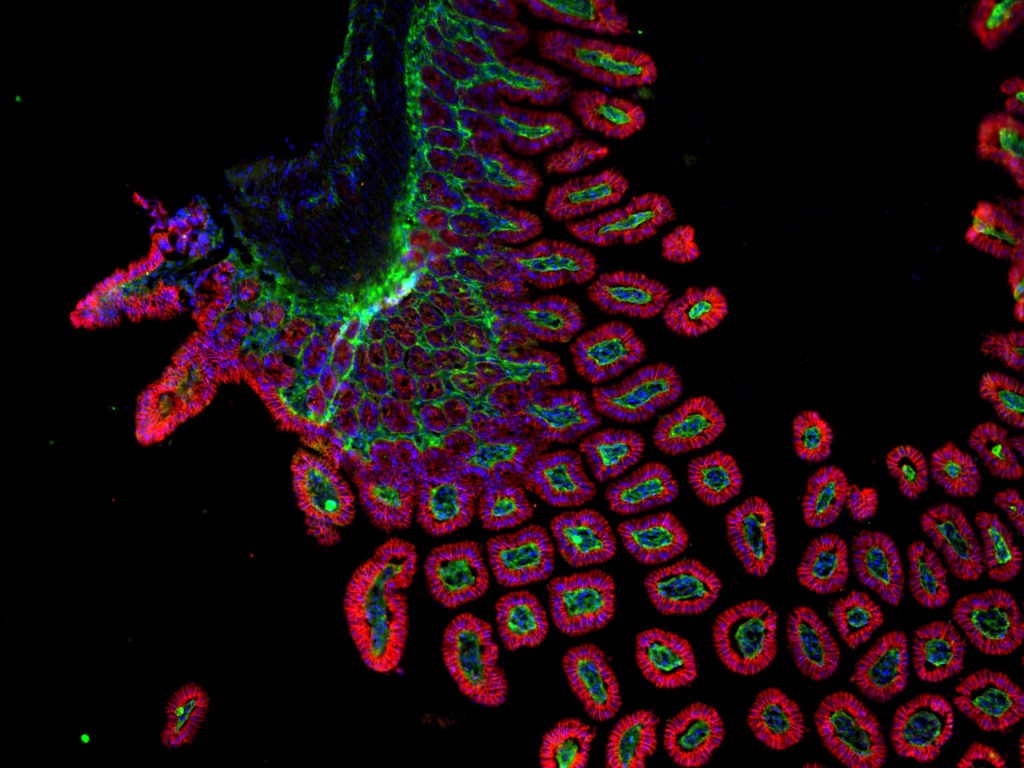
These variants were enriched in the middle of a conserved region of the non-protein coding gene RNU4-2, a small nuclear RNA (snRNA), in the NDD population dataset. Chen contacted clinicians from Genomics England to raise a clinical collaboration request to characterize the phenotypes of these individuals. Using data Genomics England had readily available, Chen and his team found that the process by which RNA gets rearranged to perform its proper function (known as “splicing”) of the RNU4-2 non-coding gene was a likely culprit of rare disease.
“This study should inspire people to look into the non-coding spaces, more generally,” Chen declared hopefully. He is pushing for more whole genome sequencing of patients with rare disease, and to do this earlier if the symptoms are more apparent. He also hopes that rare disease labs will prioritize developing methods to predict the impact of non-coding RNA variants.
Exploring rare diseases in the dark matter of DNA may reveal pathways in others’ scientific journeys to improve human health and disease outcomes. By starting at the margins, scientists can make an immediate impact. More than 10,000 rare diseases exist, affecting 30 million people in the United States. Combining science and human-centered design might just enable human-centered science to help us find answers in the most obvious of places.
Edited by Jameson Blount & Jayati Sharma



Leave a comment