Participant diversity improves genetic research for all.

Someday, perhaps 5 or 15 years in the future, you may walk into your doctor’s office for a routine check-up and walk out with a genetically tailored day-by-day diet plan, medication prescription, and exercise regimen made just for you based on your unique DNA. You will go on about your day with the knowledge that your medical plan keeps you at the lowest possible risk for chronic diseases that dominate the top 10 leading causes of death.
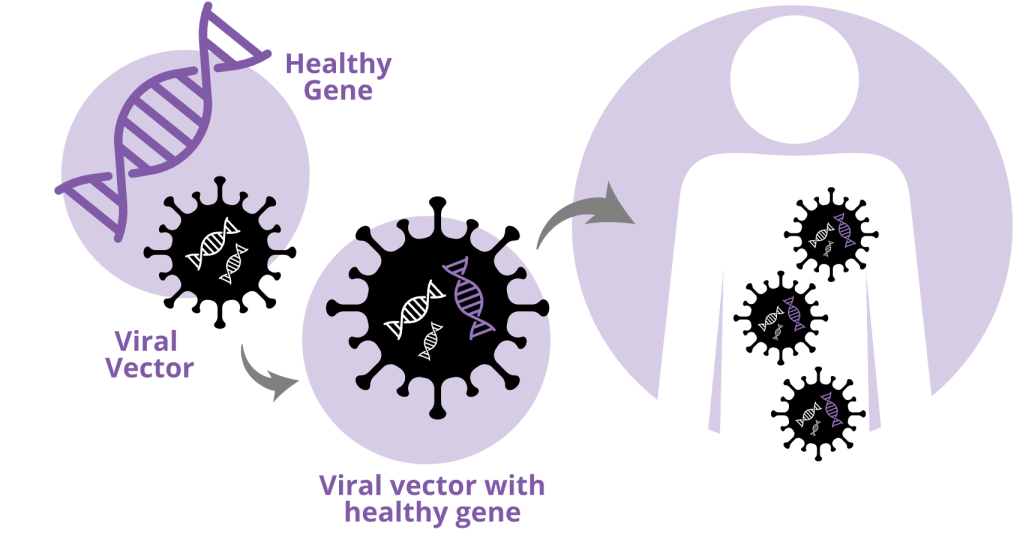
This futuristic reality, while it seems constructed out of a sci-fi film, is currently under study in many genetics and statistical labs around the world through precision medicine, which aims to use genetics to personalize healthcare at the individual level. One precision medicine technique involves polygenic risk scores (PRSs), which calculate your genetic risk for any trait of interest (diabetes, heart disease, cancer, etc.) by adding up how many of each specific risk-predicting As, Ts, Gs, or Cs, you might have at specific locations in your DNA that are known to be associated with a disease. The more of these risky genetic pieces you have, the higher your genetic risk for a given health condition may be. These risk scores don’t guarantee a future diagnosis of any condition or disease, but knowing your genetic risk for a condition can help you seek out healthier lifestyle choices to prevent it, or even pursue treatment in exceptional cases.
A noted problem with these PRSs, however, is that they are generally better at predicting genetic risk in populations of European genetic ancestry than all others. This stems from the historic exclusion of diverse populations from research initiatives and recruitment, as well as the systemic barriers that make it hard for these populations to donate their time and efforts and participate in intensive research studies. In countries like the US where minority populations bear a disproportionately high burden of disease due to structural inequities, a lack of accuracy in genetic prediction of these populations only heightens disparities. In the future, this could serve to widen the existing gaps between the health of predominantly white and that of POC (persons of color) communities in the US.
A team of over 600 researchers within the Global Lipid Genetics Consortium amassed data from over 1 million participants around the world to understand not only how to solve this problem, but prevent the social, structural, and economic conditions that might lead to it in the first place.
In their Nature study — the world’s largest genetic study of cholesterol levels to date — these researchers combined participant data from 201 studies representing 35 countries. Of the 1.6 million participants included in the study, around 300,000 represent diverse ancestry populations from African, African American, East Asian, Asian American, Hispanic, and South Asian groups. Through this Herculean scientific effort, the researchers found that the recruitment and inclusion of data from diverse populations improved genetic discovery across individuals of all genetic ancestry groups.
The performance of PRSs of LDL-C, a type of cholesterol that is a known risk factor for heart attacks, was significantly improved for all participants when diverse samples were included in the PRS compared to when data from only European ancestry individuals were used. For example, even though African ancestry participants only made up about 8% of the initial genetic analysis, their inclusion improved LDL genetic risk prediction for all ancestry groups.
Importantly, these improvements in discovery did not require an enormous representation of diverse populations, highlighting the relatively low cost and high reward of incentivizing diverse ancestry populations’ participation in genetic studies. Clinically, using these multi-ancestry PRSs would mean that you can be confident of your personalized medicine and care plans regardless of your genetic ancestry.
Cristen Willer, co-senior author of the study and Professor at the University of Michigan, shared on Twitter: “If you want to help improve the health of the people in your family, community, state, country, planet — join a genetics study! Your DNA may hold the clues to understanding health or disease to help many, many people.” And indeed, our best shot at a more equitable version of the inevitable precision medicine of the future is by contributing ourselves to the research that will be its foundation.
Edited by: Maria McSharry


Leave a comment